This post is the second in a series on working with hospital charge files. The first post in the series, How to Open and Analyze Hospital Standard Charge Files, explains what hospital standard charge files are, why hospitals are required to make this data publicly available, and how to open and analyze hospital standard charge files in a Row Zero workbook.
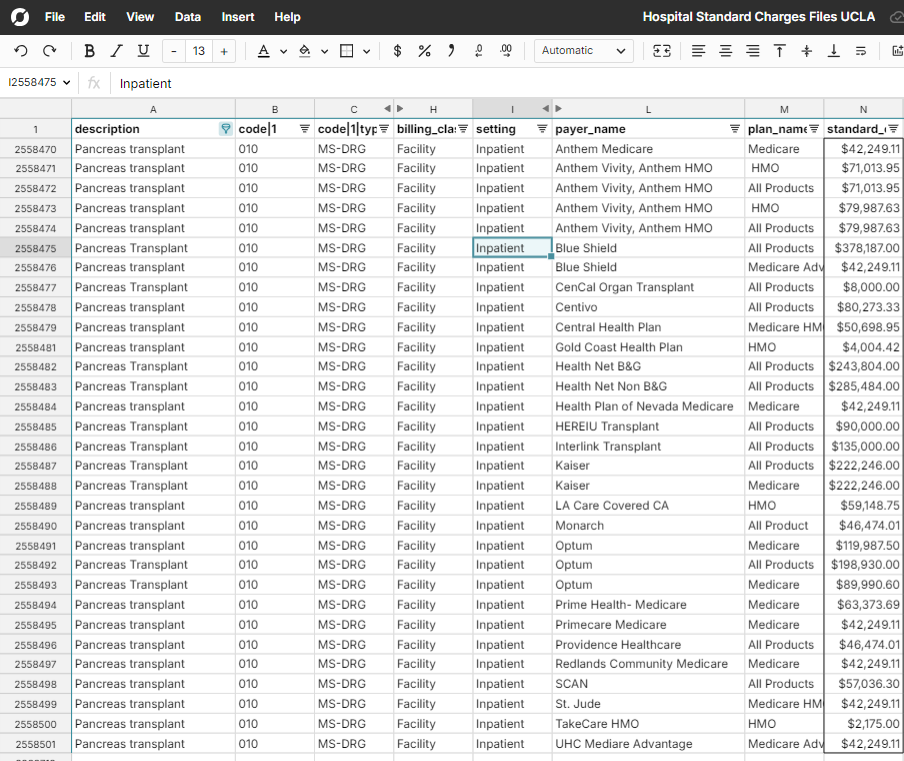
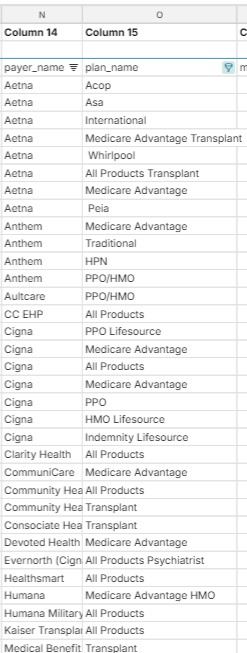
In this post, I’ll explain how to actually make sense of the data contained in hospital standard charge files. I’ll assume you’ve already downloaded and opened a file. You can check out files from hospitals at UCLA, NYU, Mayo Clinic, and Cleveland Clinic in this Row Zero workbook. Continue reading or skip to a section using the table of contents.
Table of Contents
- What is a charge and how does that relate to the actual amount paid?
- Payer-Negotiated Discount Pricing
- Payer Negotiated Charge Methodologies
- Columns and Codes
- Payers and Plans
- Setting
- Codes and Code Types
- Conclusion
Before really digging into the data contained in hospital standard charge files, it helps to know a bit about how healthcare charging and billing works and how hospitals negotiate prices with insurance companies.
What is a charge and how does that relate to the actual amount paid?
A “charge” is a dollar amount set by a healthcare system for an item or service they provide before any discounts. You’ll see this amount referred to as the “standard_charge|gross” column in hospital standard charge files. The amount that the healthcare system ultimately plans to collect for the item or service is almost always less than the gross charge amount. Before a bill is actually sent to an insurance company (referred to as a “payer” in the charge files) or a patient, a discount will most likely be applied to the charge amount.
So what are these discounts? If a patient is paying out of pocket, there is generally a self-pay discount applied to the charge amount. This amount should appear in hospital standard files as the “standard_charge|discounted_cash” column. If a patient has a government-issued insurance plan like Medicare or Medicaid, there is a standard fee schedule that the healthcare system will use to discount the charge amount before billing. If a patient has a plan through a commercial health insurance company and the hospital or provider is considered “in network” for the patient, there is generally a negotiated discount amount between the hospital and insurance company.
Payer-Negotiated Discount Pricing
So how are these negotiated prices for items and services determined between payers and healthcare systems? Generally, larger payers have more leverage to negotiate lower prices with healthcare systems because they drive a higher number of patients to the healthcare system. Negotiations can be complex and vary widely for different types of services. Eric Bricker has a great one and a half minute YouTube video that explains hospital-insurance company negotiations with some examples. Healthcare systems and payers use a lot of different charge methodologies and payment models to agree on charge amounts.
Payer-Negotiated Charge Methodologies
Sometimes, the amount that a healthcare system negotiates with a payer is just a straightforward dollar amount. This shows up in files as the “negotiated_dollar” columns. However, healthcare systems and payers often negotiate with more complex charge methodologies. Here are a few of the more common methodologies you’ll come across in hospital charge files.
Fee schedule
A fee schedule is simply a set of prices for procedures, items, and services. Government programs like Medicare and Medicaid use set fee schedules to determine prices. For charges using a fee schedule, you’ll generally see the negotiated_dollar column populated with a price by payer.
Case rate
Case rate charging is also known as “bundled charging.” Case rate charging means that all charges for a given service or procedure are bundled together and the payer pays one flat rate. Generally, case rate charging is used for procedures that have a well-defined treatment protocol without much variance, meaning they also have predictable resource utilization for the hospital.
Percent of total billed charges
"Percent of total billed charges" is a payment model where payers agree to pay a set percentage of the hospital's or provider’s full billed charges for services rendered. Instead of negotiating fixed rates for each service, the insurer reimburses a percentage of the provider's listed charges, regardless of the actual cost of care. For charges using percent of total billed charges, you’ll see the negotiated_percentage column populated with a decimal value representing the percentage paid.
Per diem
Per diem charging is a payment model where a healthcare system is reimbursed a fixed daily rate for each day a patient receives care, regardless of the specific services or treatments provided that day. The daily rate typically covers all routine services and care. Per diem rates are often negotiated with different levels of care.
Estimated Amount
If a charge uses the percentage of billed charges or an algorithm, then the hospital must provide an “estimated amount” for the charge based on historical claim data.
Columns and codes
Now that you have some idea of what a charge represents and what the various charge amounts and methodologies mean, let’s relate this all back to the structure of the hospital standard charge files. The two most common formats for hospital standard charge files are the “CSV Wide” template and the “CSV Tall” template.
Wide CSV Template
If the hospital’s standard charge file uses the CSV Wide template, a row in the file represents a charge and the negotiated charge details that the healthcare system has negotiated with different payers will appear as columns. 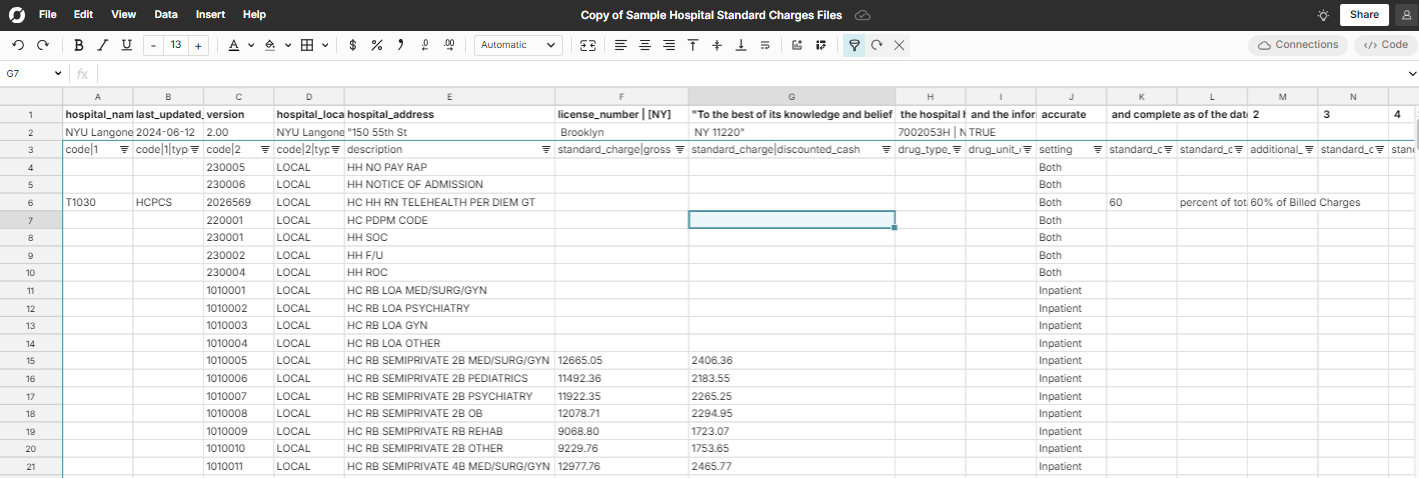
Tall CSV Template
If the hospital’s standard charge file uses the CSV Tall template, a row in the file represents a treatment, procedure, or supply. The various payer negotiated rates will appear in distinct columns. Below we clarify the other values you will see in a hospital standard charges file. 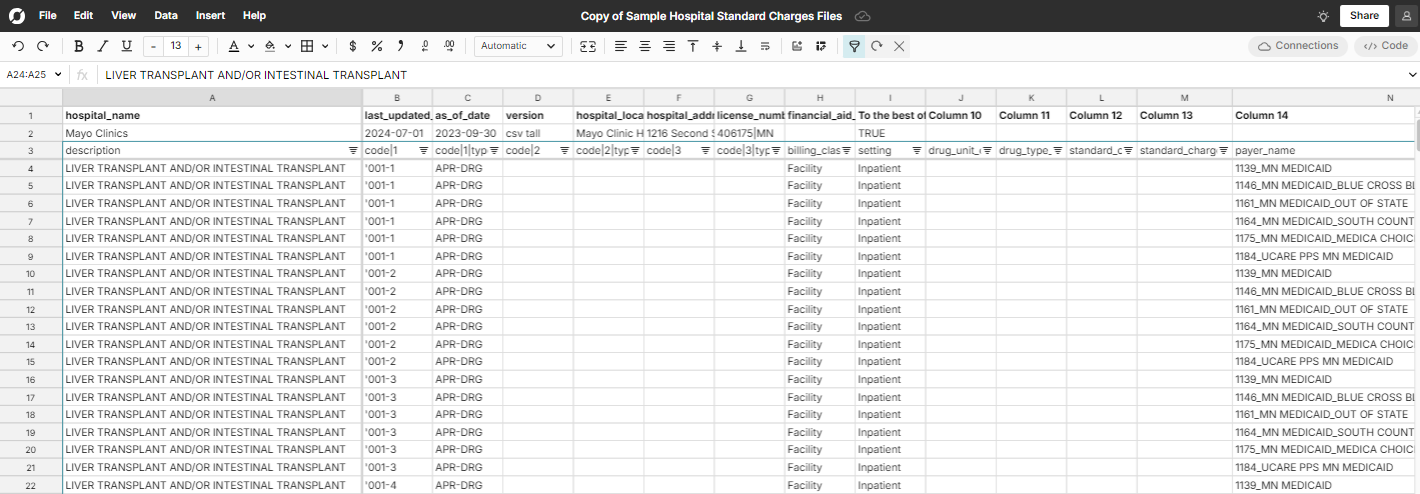
Payers and plans
Payer Name
Payer name is typically the insurance company that has negotiated the price with the hospital. Some examples are United Healthcare, University of Pittsburgh Medical Center, Aetna, etc...
Plan Name
Plan name is the insurance plan, like what you see on your insurance card. These plans might be part of government programs, like Medicare and Medicaid or could be commercial insurance products. Insurance companies often have a large number of insurance plans and there may be a large number accepted at any hospital.
Setting
The “setting” column has 3 possible values: Inpatient, Outpatient, or Both. “Inpatient” indicates that the charge is associated with patients who are admitted to the hospital. “Outpatient” indicates that the charge is associated with patients not admitted to the hospital. An outpatient charge for a service might physically take place at a hospital - it just depends if the patient is admitted or not. Inpatient charges tend to be higher than outpatient charges for similar services because hospital costs are higher for inpatient stays (and because reimbursement rates are higher). 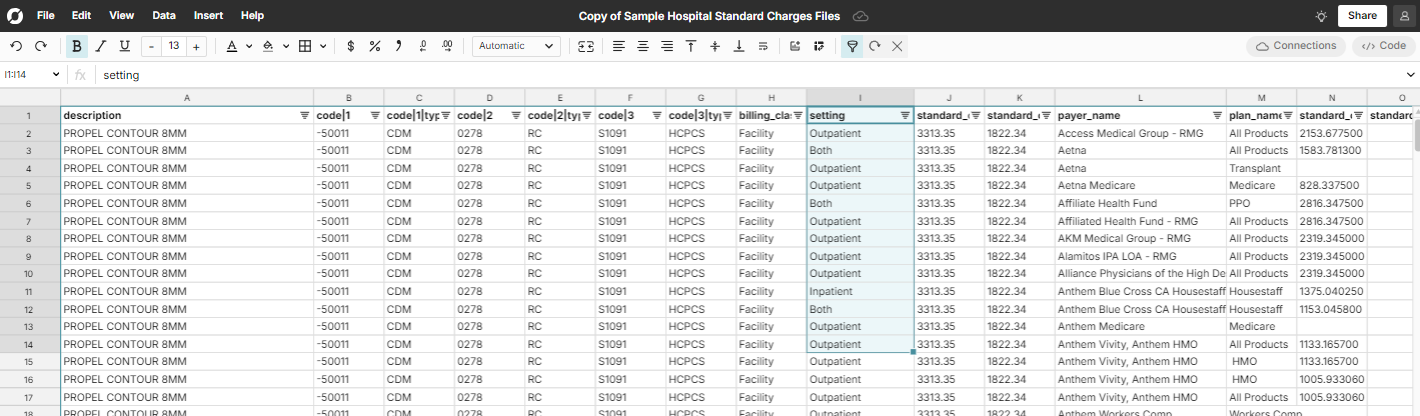
Codes and Code Types
There are a lot of different code types. I’ll cover a few of the most common ones here.
CPT
CPT stands for Current Procedural Terminology. CPT codes are a standardized set of procedures and services developed by the American Medical Association (AMA). CPT codes are divided into three categories: Category I (common medical procedures), Category II (performance measurement), and Category III (emerging technologies). They are very common codes to represent procedures performed by physicians and other providers.
DRG
DRG stands for Diagnosis-Related Group. You’ll see many variations of DRG codes, like AP-DRG, MS-DRG, etc. All of these code types are based on the same idea. DRG codes are a classification system used in healthcare to group patients with similar clinical conditions and resource usage, primarily used in hospital billing for inpatient services. DRG codes are used widely in government payment systems, like Medicare and Medicaid. Each DRG is assigned based on factors such as the patient’s diagnosis, procedures performed, age, and other medical conditions.
CDM
CDM stands for Charge Description Master. CDM codes are specific to a hospital and can be thought of as an internal code for all billable services and procedures the hospital offers. The main thing to note here is that unlike many of the other standardized code types, CDM charges are difficult to compare like-for-like across hospital systems since each healthcare system’s charge description master coding system is unique.
NDC
NDC stands for National Drug Code. NDC codes are unique identifiers assigned to medications approved for sale in the United States and managed by the FDA. NDC codes are used to identify the drug manufacturer, product, and packaging. The code is divided into three segments: the labeler code (manufacturer or distributor), the product code (specific drug and strength), and the package code (size and type). In addition to NDC codes, for drug charges, you’ll also see drug_unit_of_measure and drug_type_of_measure columns populated. These columns are particularly helpful when comparing drug charges across hospitals.
Conclusion
Hospital standard charge files are publicly available for all hospitals in the United States and contain an immense amount of data. You can use them to understand how much healthcare systems charge for various items and services, how healthcare systems negotiate prices with payers, and how charges vary across different healthcare systems. Understanding the basics of how healthcare systems negotiate with payers, how different charge methodologies work, and what common hospital coding systems represent gives you the basic knowledge you need to start analyzing hospital standard charge files. The CMS GitHub site also has good documentation to help make sense of these files. To view a standard charges file for yourself, check out our blog on how to open hospital stnadard charges files.